Candida albicans: Types of Infection & Natural Treatments
What do the vast majority of the global population have in common? There are almost 8 billion of us alive at this moment in time, so what could be the shared among 6 billion people?
You may be surprised to find out that the answer is fungi! One particular fungus in fact; Candida albicans.
Most people are never aware that they are home to a range of bacteria, yeasts, and fungi.
Most of these microorganisms are commensal, meaning that they exist in harmony with us and do not cause any detrimental health effects. Others are pathogenic, meaning that they cause disease.
Your body is in a constant state of flux; a battleground between your immune cells and these disease-causing agents.
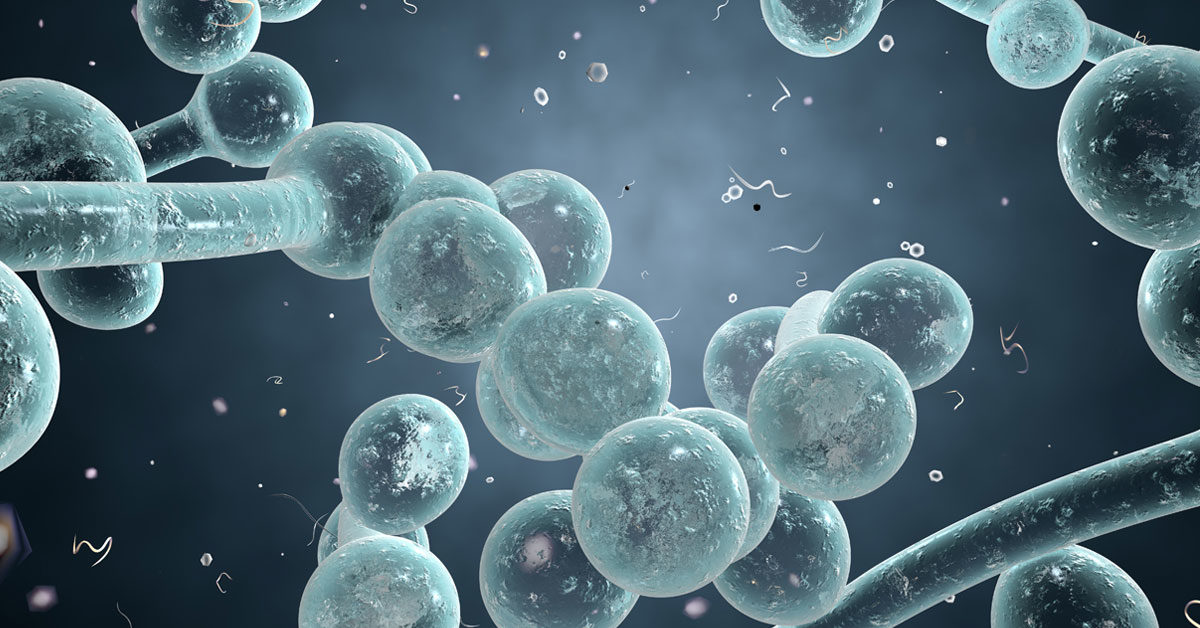
Candida albicans is both a natural commensal fungus and a fungal pathogen. Fungi with one just one cell are classified as yeasts and Candida fits this bill. However, it is a fascinating fungus because it can also be classified as hyphae due to its ability to grow in a branching manner.
Complications occur when your immune system is not functioning optimally, presenting a window of opportunity for Candida and other potential pathogenic microbes to multiply beyond their regular parameters. It is this multiplication that throws off the delicate balance of your microbiome and can lead to the signs of Candida overgrowth.
You have probably heard of thrush, or perhaps even suffered the uncomfortable and itchy condition yourself. Thrush is a frequent presentation of Candida overgrowth; however, the effects of Candida can be numerous and varied. An intestinal Candida overgrowth can lead to a wide range of symptoms across your body.
Table Of Contents
What is Candida Albicans?
The short answer is that Candida albicans is a fungus that can be found in the digestive tract or elsewhere on your body. However, that is not all there is to this microorganism. Let’s dive deeper and find out more about this fascinating and sometimes destructive fungus.
Fungus, yeast, or hyphae?
You may have heard of the term’s fungus and yeast, but what about hyphae? What is the connection to Candida?
The definition of a fungus is a spore-producing organism. The fungus family feeds on organic matter, and they include molds, yeast, mushrooms, and toadstools.
Yeast is a type of single-cell fungus, which means that it consists of one oval cell. It reproduces from itself by budding off new single-cell fungi.
Hyphae are the long, branching filaments that enable a fungus like Candida albicans to grow and spread. These hyphae are not present when Candida is in its yeast form.
Candida is an unusual fungus. It was initially deemed dimorphic, meaning that it has the ability to grow as a yeast or hyphae. However, it is now labeled as polyphonic, meaning that different phenotypes can arise due to differences in the surrounding environment. This is also referred to as phenotypic plasticity.
In short, this means that Candida is a shapeshifting fungus that can adapt to whatever environment in which it finds itself.
What does this mean for the human body?
Pathogenic or disease-causing fungi use the hyphal form of growth to invade tissues in the body and then enter the bloodstream. The hyphal form of growth and development is, therefore, more virulent than the single cell yeast form.
In its non-pathogenic yeast form, Candida exists as a single-cell yeast. When environmental changes enable it to change to its hyphal form, it can begin to cause health problems in the gut and elsewhere.
A commensal organism
Candida is a commensal fungus, meaning that it resides typically on and within your body in both your tissues and in bodily fluids including saliva, blood, and urine. (1)
Under normal circumstances, Candida does not cause any damage or detriment to your health. Your skin, genitals, mucus membranes, and intestines can all have Candida without causing any significant health issues.
Candida quietly survives by utilizing the broken-down components of sugar and other nutrients to give it the energy to reproduce, and yet living in harmony and balance with your body. Most of the time, it forms part of a normal and healthy microbiome.
How do we acquire Candida albicans?
There are a number of ways in which Candida can populate your microbiome. It is now believed that the majority of us become colonized with this fungus during the birthing process from our mothers, and it remains with us throughout our lives. (2)
If you are in the minority and do not become colonized with Candida from birth, it is likely that you will become so later on in life through contact with another human who has Candida as part of their microbiome.
Hospitals are exceptionally efficient places at passing on Candida. If you were to be admitted to hospital and were negative for Candida, there is a significant 40% chance that you will leave the hospital with Candida. As a rule, it is transmitted from hospital employees to the patients. (3)
Why is Candida albicans difficult to treat?
Candida can be somewhat of a tricky customer. Yes, it forms part of your microbiome and can live with you peacefully for decades. However, when a Candida overgrowth occurs, it can be challenging to overcome.
There are several reasons why Candida is so awkward to treat. Below are four of the strategies that Candida employs to protect itself from your immune system.
Biofilms
As you know, Candida can exist as a “friendly” member of your microbiome, or it can behave as a pathogenetic fungal invader.
Candida increases its pathogenicity by creating a biofilm which acts to shield it from your immune system and medications, including antifungal drugs.
Nature produces a range of biofilms. You are probably familiar with the slime that you can find on rocks in ponds and streams, or even that unpleasant film that you see on your teeth in the morning.
These are biofilms; communities of microorganisms that attach themselves to a surface. The bacteria or fungi excrete a sticky, sugar-rich substance that covers them and creates a matrix which is referred to as a biofilm.
A biofilm is in effect an additional layer of protection for the microorganisms that it covers. The biofilm is made of extracellular polymeric substances (EPS) that are produced by the microbes. The EPS forms sticky strands that form the mesh that is at the core of the biofilm, and that sticks to both exterior surfaces and the microbes within the film.
How effective the biofilm is depends on how competent the bacteria or fungus is at producing this EPS. Amongst Candida species, there is great complexity and diversity of EPS production.
It is these differences in EPS that allows Candida albicans to form stubborn colonies that have high levels of antifungal medication resistance and that act as resilient barriers to drug diffusion. Both of these factors mean that antifungal drugs show lower efficacy or even total ineffectiveness. (4)
Determining new methods to circumnavigate the biofilm produced by Candida is proving to be a significant challenge.
Yeast-to-hyphae switching
Dimorphic switching is a complicated sounding term, but it simply means that Candida can switch between yeast and hyphal form.
Candida is an excellent survivor and can cope with a wide range of environments because it senses its surroundings and then adapts to them. It is this ability to switch that makes Candida such a formidable pathogen. (5)
Candida grows as oval shaped yeast cells; however, it has the ability to shift to hyphae if the available nutrients, temperature, pH level or CO2level demand it.
These two types of cell behave in different ways. The oval yeast cells are best at entering the bloodstream, whereas the hyphal cells increase the virulence of Candida in invading and penetrating tissues, establishing colonies in the organs and in avoiding your immune cells. (6)
An excellent shapeshifter, Candida also has another form, the chlamydospore. Candida in this form is spherical, smooth, and multicellular. Scientists do not fully understand the purpose of the chlamydospore, but it is thought that Candida alters new growth to this form in order to survive harsh environments. It can be induced in the laboratory under unfavorable conditions, but it is rarely seen on living beings. (7)
Genetic Diversity
Candida reproduces asexually, creating a new yeast cell from its own genetic material. However, in some circumstances it can also fuse with another Candida cell. When this occurs, genes between the chromosomes can be exchanged.
This means that Candida can display wide genetic diversity across the population, leading to different types of infections that are better at adapting to changes in their environment. (8)
Altering the pH of its surrounding environment
The acidity or alkalinity of a substance can be measured by pH. The value can be from 1 to 14; the more acidic the solution, the lower the number. A neutral pH is 7.
The human body goes to great lengths to ensure that the bloodstream is always maintained at a slightly alkaline pH of 7.4. Breathing, drinking, urinating, and other bodily processes regulate this delicate balance. However, the stomach has a pH of 2-4; the colon has a slightly acidic pH of 5.5-7 and the vagina around pH 4.5.
Candida albicans shares our need for a neutral environment, and its ability to adapt to pH is large part of its virulence.
Candida has developed a rapid way to alkalize any acidity that it detects. It excretes ammonia from its cells, which has the ability to raise the local pH from 4 to more than 7 in just twelve hours. The Candida is then triggered to switch to the hyphal form from the yeast form, which in turn increases its virulence. (9)
Candida can hide from your immune system
Candida albicans is able to play a destructive game of hide and seek with your immune system by making changes to its cell walls so that it can escape detection.
You are born with an innate immune system that recognizes invaders into your body. Pathogens have proteins called antigens on their surface, which show your immune system which cells they need to attack.
Your immune system uses a system including special sensors called Pattern Recognition Receptors (PRRs). They allow your immune system to figure out precisely whether the invader is a fungus, virus, or bacteria, and decide on the most appropriate immune response.
Candida cell walls consist of a matrix of α- and β-mannans. The β-glucan on the fungal cell wall is recognized by your immune system. This triggers a process known as phagocytosis, where the immune cells neutrophils and macrophages consume the pathogen. (10)
It is this process of phagocytosis that Candida has managed to avoid. It hides the β-glucan on its surface, thereby removing the ability of your phagocytes to recognize and destroy invading Candida cells.(11)
As you can see, Candida is exceptionally good at adapting itself to evade your immune system.
Common Types of Candida Infection
Candida infections can also be referred to as candidiasis or thrush, and they can occur in a variety of places on the human body. Some of these complaints are very common. For example, 3 out of 4 women will experience vaginal candidiasis at some point in their lives.
Those with impaired immune systems are more likely to suffer from Candida overgrowth, as are the elderly and very young. (12)
Other factors, such a high-sugar diet or antibiotics, have also been linked to an increased change of Candida infection.
Here are the 4 most common types of Candida infection.
Vaginal yeast infections
Yeast infections are also referred to as vulvovaginal candidiasis (VVC). They are experienced by around three quarters of women. Half of these women will have repeat yeast infections, and 5% will suffer from recurrent yeast infections with four flare-ups or more annually. (13)
Yeast infections can become stubborn and chronic and lead to sexual disfunction in extreme cases.
Causes
Candida albicans causes VVC in over 90% of cases, although there are other culprits including Candida glabrata, Candida tropicalis, Candida krusei, and Candida parapsilosis.
Candida is part of the natural microbiome of the vagina and vulva. However, when a woman becomes pregnant, uses antibiotics, takes oral contraceptives, or has diabetes, the Candida can become pathogenic and overgrow, causing the symptoms of VVC.
Symptoms
The symptoms of VVC typically include:
- Itching of the genital area
- Soreness
- A white, curd-like discharge
- Vulvitis, or inflammation of the vulva
- Vaginitis, or inflammation of the vagina
- Swelling
- Pain while urinating
- Pain during sexual intercourse
Treatment
There is a range of over the counter antifungal creams, vaginal pessaries, and oral medications that can be used to treat VVC.
There are other possible causes behinditching and vaginal discharge, such as sexually transmitted infections or bacterial vaginosis, so make sure that your VVC has been diagnosed correctly. (14)
Natural treatments
Using a quality probiotic supplement will help to keep your microbiome balanced and healthy. Foods that are rich in probiotic bacteria, including yogurt, will also help to support this balance.
Reducing or eliminating the amount of sugar in your diet will help to restrict the food source of Candida, and lower the risk of yeast infections.
Topically applied yogurt and coconut oil are both soothing and active against VVC.
Prevention
Behavioral changes can help to prevent VVC.
- Wear loose clothing to encourage airflow
- Do not use synthetic underwear
- Wash your hands after using the toilet
- Always wipe yourself from the front to the back, never the reverse
- Avoid soaps and sprays including deodorant, in the genital areas
- Minimize antibiotic use
- Wash underwear in hot water to kill any fungus
- Optimal control of blood sugar if you are diabetic
Oral thrush
Also called oral candidiasis, oral thrush is an overgrowth of Candida in the oral cavity. Usually, there are visible patches of white thrush on gums, palate, tongue, tonsils, and throat
Candida albicans often lives in the mouth without causing any ill effects, However, in the right circumstances it can grow out of control.
This form of candidiasis is not particularly common in healthy adults. It is more widespread in the young and elderly, and those with weakened immunity.
Symptoms
During the initial stages of infection, you may not notice the signs of oral thrush. With progression, you may see the following indications of candidiasis:
- Patches or lesions of creamy white fungus most usually seen on the tongue and inner cheeks and sometimes on the gums, tonsils, and throat.
- A burning or painful sensation which can cause difficulty in swallowing or eating.
- Bleeding
- Cracked and red skin in the corners of the mouth
- A loss of taste
In those with weakened immunity, the infection can continue into the throat and can cause pain and a sensation that food is continuously stuck in the throat.
Treatment
Your doctor might prescribe oral fluconazole or clotrimazole lozenges. Nystatin mouthwash can be used in adults or swabbed around the mouth in the case of babies. Itraconazole and amphotericin is used to treat stubborn and severe cases.
Natural treatments
Thankfully there a range of natural remedies for the treatment of oral thrush.
- Drinking cranberry juice, sugar-free of course! This increases the acidity of the mouth and makes it more hostile for Candida albicans to grow.
- Using coconut to swish around the mouth has been shown to rid the mouth of undesirable microorganisms. (15)
- Oregano oil is antifungal, antiviral, and anti-inflammatory. Use a few drops of this powerful natural oil, diluted in water, as a mouthwash.
Urinary Tract Infections
Bacteria usually cause UTIs but, in the last 25 years, the proportion of UTIs caused by Candida has increased significantly.(16)
Causes
As with other Candida albicans infections, the likelihood increases with weakened immune function.
Certain factors make a Candida UTI more likely, including being female, pregnancy, urinary stones, urologic structure abnormalities, diabetes, hypertension, and instrumental catheterization.
Symptoms
These are the same with both bacterial and candidal UTIs. Generally, patients are found to have a Candida infection when their UTI does not respond to standard therapy, and a culture is taken.
Symptoms include:
- Painful urination with a burning sensation
- Needing to urinate more frequently than usual
- Pain or pressure in the pelvis and lower abdomen
- Urine that is cloudy, dark, bloody or unpleasant smelling
- Fever if the infection becomes more severe and affects the kidneys
Treatment
Oral antifungals are the treatment of first choice, namely fluconazole, because it is capable of reaching high concentrations in the urine. (17)
Using probiotics and fermented foods can help the body to rebalance the microbiome and to recolonize the urinary system with friendly organisms. It’s a good idea to add kefir, kimchi, sauerkraut, and kombucha to your diet. (18)
Candida infections on the skin
Cutaneous candidiasis is when Candida overgrowths affect the skin, causing diaper rash, nail fungus, and athlete’s foot depending on where the candidiasis is located.
Candida albicans exists in a healthy skin microbiome. It is only when the conditions are right, that it overgrows and causes irritation.
Causes
Candida loves to grow in warm and moist conditions. Diapers, nail beds, folds of skin, the groin, and your sports shoes provide the ideal conditions for it to multiply.
Nursing mothers can pass Candida back and forth between the oral cavity of the baby and their own skin.
Obesity, poor hygiene, tight, synthetic clothing, excessive perspiration, antibiotic use, and a weakened immune system can all make a Candida overgrowth more likely.
Symptoms
A rash might be the first symptom that you notice, accompanied by itching. As the rash progresses, the skin might crack and become painful. There may be small blisters and pustules present.
Candidiasis may be mistaken for another skin condition, including dermatitis, eczema, psoriasis, ringworm, herpes, or hives.
Treatment
In mild cases, merely adhering to a good hygiene regime may be sufficient to overcome the condition. Changing diapers, socks, and clothing more frequently can help. Antifungal skin creams are the next step if the Candida persists.
Using tea tree oil at a low dilution, coconut oil and apple cider vinegar are all-natural treatments that have been proven to be useful for the treatment of cutaneous candidiasis.
Intestinal Candida overgrowth
When the delicate balance of your gut microbiome becomes off balance, through illness, antibiotic use, or even stress, Candida can proliferate and can cause the uncomfortable indications of an intestinal Candida overgrowth.
Causes
With perfect health, an overgrowth of Candida is unlikely. Candida may seize the window of opportunity that comes with a compromised immune system. There are other causes:
- Using antibiotics
- Drinking alcohol
- Using oral contraceptives
- Uncontrolled diabetes
- Stress
- A poor diet that is high in sugar and refined carbohydrates
Symptoms
Initially, your symptoms may be unspecific. Unexplained tiredness is a frequent symptom. Candidiasis often affects how your body absorbs nutrients so you might suffer from deficiencies in magnesium, essential fatty acids, and vitamins. Nutritional deficiencies can lead to fatigue. (19)
A study has shown that under certain circumstances, intestinal Candida overgrowth could cause chronic fatigue syndrome. (20)
The gut microbiome is essential to your digestion and the processing of some sugars, fiber, and starch. When Candida proliferates, you might experience digestive problems, constipation, nausea, cramping, gas, diarrhea, or bloating.
Chronic and severe digestive diseases, including Crohn’s disease and ulcerative colitis, have been associated with intestinal Candida overgrowth. (21)
Treatment
To overcome an intestinal Candida overgrowth, there are three necessary steps; stop the growth of Candida, restore the balance of the gut microbiome, and heal the gut so that Candida cannot enter the bloodstream.
Traditional medical approaches focus solely on stopping the growth of Candida, which can be achieved with antifungal drugs. A more holistic approach is needed to tackle Candida in its entirety.
Limit the carbohydrates and sugars in your diet to starve the Candida. Help your microbiome to rebalance by taking a quality probiotic. And heal your gut by eliminating inflammatory foods such as red meat, and reducing your intake of alcohol and unhealthy, processed foods.
Less common types of Candida infection
Candidiasis can take many forms, some more serious than others. Thankfully the more severe conditions are rare but are potentially lethal.
Candidemia
When Candida enters the bloodstream, it can cause serious problems that can even become life-threatening. The Center for Disease Control estimates that there are 25,000 cases of candidemia, an infection of the blood caused by Candida, every year. (22)
Candidemia is extremely rare in healthy individuals; however, people suffering from neutropenia or low levels of neutrophils in the blood are at risk. Neutropenia widely occurs following chemotherapy and radiation therapy for cancer or other bone marrow diseases.
Risk factors
Those who have a serious underlying health condition are far more likely to suffer from candidemia. The following conditions make candidemia an increasingly likely diagnosis:
- Major surgery
- Immunosuppression through HIV, cancer, and chemotherapy, or steroid use
- Use of broad-spectrum antibiotics
- Catheterization or placement of a feeding tube
Symptoms
Candidemia can be mistaken for bacterial sepsis due to similar symptoms, which include kidney failure, fever, and progress into shock.
Treatment
Following a blood test diagnosis of candidemia, the patient will be started on intravenous dosing with fluconazole, micafungin, or caspofungin. Treatment may be for extended periods depending on the individual and their response.
Endocarditis
An extremely grave condition with a high likelihood of mortality. It is an infection of the inner chambers and valves of the heart. Candida albicans is the causal agent in a quarter to half of all fungal endocarditis.(23)
Risk factors
- Cardiovascular surgery
- Heart abnormalities and defects
- Immunosuppression through HIV, cancer, and chemotherapy, or steroid use
- Prolonged use of broad-spectrum antibiotics
- Prosthetic heart valves, catheterization or placement of a feeding tube
Symptoms
Fungal endocarditis and bacterial endocarditis manifest themselves in a similar manner. There can be general systematic indications, including body pain, cough and fever, and more localized symptoms, including chest pain and difficulty breathing.
Treatment
If a medical device is fitted, this should be removed, and the heart may require surgical excision of the infected tissue. Intravenous fluconazole or amphotericin B are the first-choice medications.
Endophthalmitis
Candida can cause this inflammatory condition of the eye. It can lead to loss of vision.
Risk factors
- Recent surgery or hospitalization
- Immunosuppression
- Having a medical device fitted
Symptoms
There may be pus and stickiness of one or both eyes. The eyes may be inflamed and red. Endophthalmitis is frequently diagnosed as a bacterial infection in the first instance.
Treatment
Antifungal eye cream, including amphotericin B with flucytosine. Fluconazole could be used.
Meningitis
If Candida enters your bloodstream, it can travel through the spinal cord and cause inflammation in the meninges, which are the tissues that surround the brain.
Risk factors
- Immunosuppression
- Hospitalization
- Surgery
- Corticosteroid or antibiotic use.
Symptoms
Bacterial meningitis and meningitis caused by Candida manifest themselves in similar ways:
- Nausea and vomiting
- Headache
- Painful and stiff neck
- Fever and confusion
- Sensitivity to light
Treatment
If meningitis does not respond to standard treatment, the cerebral spinal fluid should be cultured to confirm Candida and intravenous amphotericin B with flucytosine will be used.
Candida Resistance to Antifungal Drugs
Human lives are greatly affected by fungi. There is, unfortunately, a growing resistance to antifungal medication in both Candida albicans and non-albicans forms of Candida.
Candida is an excellent evader of the immune system and can rapidly develop the ability to resist and defeat the medication that is designed to kill them, which means that the infections that it causes are challenging to treat and cure. (24)
How much of a problem is antifungal resistance?
In Candida that is isolated from the human bloodstream, around 7% of the samples are resistant to fluconazole, which is the drug of first choice for numerous forms of candidiasis. (25)
For Candida that is resistant to fluconazole and to echinocandin, there are few treatments available. Amphotericin B is a medication that can be used, but it is also a toxic drug that could endanger the life of a patient who is already at risk. (26)
What causes antifungal resistance?
As with antibiotic use, resistance can occur over a period of time. Frequently this is due to antifungals being misused, which happens when patients self-medicate or do not follow the instructions of their physician. If antifungals are not used at the correct dosage or the course is discontinued prematurely, the fungus can evolve to be resistant to the antifungal. (27)
It is not just the use of antifungal medication that can induce resistance. Antibacterial drugs can also play a part. Your microbiome is perfectly balanced when you are healthy, and antibiotics shift this balance by reducing the number of good bacteria in the gut and allowing Candida to multiply. Care should be taken when using antibiotics. Only take them when absolutely necessary, and it is prudent to employ the use of probiotics concomitantly. (28)
What can you do to reduce antifungal resistance?
Do not use antibiotics or pharmaceutical antifungals unless it is absolutely necessary. If you do take them, ensure that you take them exactly as prescribed, at the correct dose and take the full course.
If you self-medicate and the condition is not improving, see your doctor to ensure that you are using treatment for the appropriate condition.
Maintaining a healthy microbiome is a massive step towards ensuring that you do not need to use antifungals and antibiotics. Choose a quality probiotic to support your health and follow a diet that naturally helps you to combat an overgrowth of Candida.
How do you treat Candida albicans naturally?
With increasing concerns on resistance to traditional antifungal drugs, treating Candida through natural means is becoming more widespread and eliminates any potential side-effects that could be observed with prescribed medications.
Treating intestinal Candida is often the most important step in eliminating a Candida overgrowth that is present in other areas of the body. That’s because the gut acts as a ‘reservoir’ of Candida that can then re-infect other areas, even after they have been successfully treated.
The importance of the correct diet
With most types of Candida infection, external or internal, the foundation of treatment lies with a low-sugar and anti-inflammatory diet plan. Candida loves nothing more than to feast on glucose; therefore, it makes sense that if your body has low levels of glucose, Candida does not have the energy source to overgrow and become detrimental to your health.
Gut dysbiosis or an unbalanced microbiome can be the cause of many conditions and general malaise.
You should avoid foods that contain sugar, such as candies, cakes, pastries, and regular soda. Be careful with foods that look like they don’t contain sugar, but it could be hidden. Processed meats and other processed, savory foods often contain sources of sugar. Also, avoid refined carbohydrates, including white bread and pasta as these are quickly broken down into simple sugars when your body metabolizes them.
Probiotics
There is a range of fermented foods that you can add into your diet to help the balance of your microbiome; these include sauerkraut, kimchi, live yogurt, and kefir.
Taking a probiotic supplement in the form of a pill or capsule is a much more convenient way to ensure that your microbiome is optimal. Probiotics contain beneficial bacteria. This is an especially good plan of action if you have had a less than ideal diet or following a course of antibiotics. Probiotics will assist your microbiome to regain balance and bring your body harmony.
There is a vast range of probiotics to choose from, and you should consider carefully which ones are a wise investment. The bacteria in the probiotic need to reach your gut, so select one that uses BIO-tract time-release technology. A BIO-tract probiotic will be more likely to deliver its bacteria to your gut.
Also examine the total colony forming units (CFUs); look for a minimum of 10 billion CFUs to be sure that the probiotic will deliver a useful number of live bacteria to your gut. (29)
Treating topical infections
Candida causes skin infections. These can be treated topically, by application to the skin or systemically, through your diet.
Try to include the following foods in your diet to help your skin to maintain health or to recover from an illness:
Oily fish
Tuna, trout, salmon, mackerel, and herring are high in protein and omega-3 fatty acids which improve skin health and help to keep it supple and hydrated. If you notice that you have dry, flaky skin, you might have an omega-3 fatty acid deficiency. (30)
Oily fish contains zinc, which you need to produce new skin cells; a deficiency can cause skin inflammation and lesions.
Fruit and vegetables
They are essential for your health. Fruit and vegetables should be the main part of your diet. Include avocados for vitamin E and C and healthy fats, which makes your skin supple and resistant to pathogens. (31) Broccoli contains carotenoids which shield you from oxidative damage leading to wrinkles and dryness. Walnuts contain essential fatty acids, zinc, and antioxidants vitamin E and C and selenium, which help your body to overcome disorders.
Topical skin applications
A lot of foods that you may already have in your kitchen can be used topically to rid your skin of Candida. Coconut oil, cinnamon oil, and olive oil are excellent choices of skin moisturizers that contain ingredients that can kill Candida. If you can stand the smell, crush up raw garlic, and apply to the affected area. Garlic is a potent antifungal agent. (32)
Foods that can kill Candida
Adding foods to your diet that can kill off Candida is an excellent way to prevent any overgrowths from occurring.
Coconut oil
In a study performed on mice that were fed either coconut oil, soya oil or beef tallow, those that were fed the coconut oil had much lower colonization levels of Candida. Coconut oil was shown to reduce preexisting colonization. Coconut oil contains the fatty acids decanoic, and dodecanoic acids, which can inhibit the growth of and kill Candida. (33)
Olive and cinnamon oil
The search for alternative treatments to antifungal resistant Candida strains is ongoing. Research has found that both olive oil and cinnamon oil are highly competent at killing Candida that was isolated from infections in the bloodstream. Over half of fluconazole-resistant Candida krusei strains were found to be sensitive to olive and cinnamon oil. (X)
Pau D’Arco
You may not have heard of this plant that is native to South America, but it has been used in traditional medicine for hundreds of years due to itsantifungal, antimicrobial, anti-inflammatory, antiviral, and anti-parasitic effects. (34)
Pau d’Arco contains the chemicals lapachol and beta-lapachone, which can kill a variety of bacteria, fungi, viruses, and parasites.
Research has demonstrated that lapachol is a powerful antifungal agent against Candida, similar to pharmaceutical alternatives. Pau d’Arco is able to disrupt the cellular membranes of Candida. (35)
Take Pau d’Arco as a tea made from the plant, or as capsules.
The Bottom Line
Candida forms part of the microbiome in your digestive system, skin, and other areas. In the majority of people, it can be a part of a healthy microbiome and cause no problems or illnesses.
Issues with Candida can arise when there is a change from the balanced and healthy state of the body. The reasons for this change could be due to the use of medications such as antibiotics or corticosteroids, stress, a change in hormone balance or an underlying disease including cancer or HIV which weakens the immune system.
When the delicate balance of the microbiome is upset, Candida takes this opportunity to grow out of control and can cause problems ranging from fatigue and poor digestion to more severe conditions such as candidemia and infections of the internal organs.
Eating a diet low in sugar and carbohydrates and taking a high-quality probiotic will help to support your immune system and keep your microbiome in balance. These measures will help to prevent any issues with Candida and the unpleasant compromises to your health that it can cause.

3-Month Candida Elimination Kit Start Your 3-month Candida Cleanse
This Candida Kit contains all the supplements recommended on the Candida Diet:
- LIVER ONE to process and remove the toxins created by Candida.
- CANDASSIST to inhibit and weaken the Candida colonies in your gut.
- PROBIOTIC to replace the Candida yeast with probiotic bacteria.
Plus... the CANDIDA DIET RECIPE BOOK with 50+ low-sugar recipes

Leave a Reply