How Does Candida Change Your Gut Flora After Antibiotics?
Candida overgrowth (or Candida Related Complex) is sometimes dismissed by the medical community as an unproven, undiagnosable condition. However, nothing could be further from the truth. The fact is that there are thousands of research papers looking into Candida albicans and the various ways in which it affects us.
Some of these papers look at topical Candida, or infections in immuno-compromised patients, but others help us to learn more about the way that Candida can colonize the gut and lead to the many, diverse symptoms of Candida overgrowth.
One such paper was published a few months ago, and it gives us a crucial insight into how Candida albicans can attain a dominant position in the gut flora soon after a course of antibiotics. This is of course one of the reasons why I recommend taking probiotics during and after your course of antibiotics. It also helps to explain why antibiotics are one of the major causes of Candida, and why using them inappropriately can have serious long-term consequences for your health.
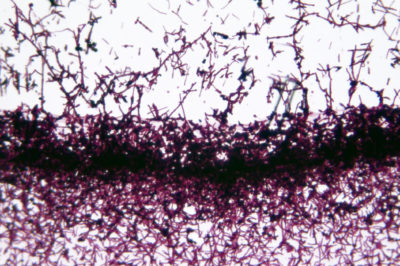
Candida albicans is an extraordinarily adaptive and opportunistic organism. For example, it can survive in both acidic and alkaline conditions, and indeed its own metabolites (byproducts) actively change the pH around it to allow for faster proliferation. (1) We know that it creates biofilms to protect itself from your immune system. And now, thanks to a study published in Scientific Reports in 2013, we can see that Candida albicans also alters the way that the gut flora is reassembled after a round of antibiotics. (2)
Table Of Contents
Antibiotics Allow Candida Albicans To Dominate The Gut
In the 2013 study, a group of female mice were treated with a broad spectrum antibiotic (cefoperazone) for 7 days. They were then inoculated with Candida albicans, and their gut flora was tested 7 days and 21 days after inoculation. Another group was inoculated with Candida albicans without a course of antibiotics.
The first thing to note is that Candida albicans effectively colonized the guts of those mice which had had been given antibiotics, and whose gut flora had therefore been significantly disturbed. In fact, the Candida colonies in these mice were still evident after a full 90 days. On the other hand, the mice with a healthy gut flora (i.e. no antibiotics) were able to fight off the Candida much more effectively. After 21 days, these antibiotic-free mice had totally eliminated Candida albicans from their guts.
Remarkably, it only took a very small amount of Candida albicans to infect and colonize the guts of the mice who had taken antibiotics. Now, Candida albicans is not usually present in mice, but it exists in the intestines of something like 70-80% of humans. Although this study was conducted on mice and not humans, it is easy to see how a course of broad spectrum antibiotics might enable the Candida colonies to quickly bloom and dominate the gut.
Candida Changes How The Gut Flora Recover After Antibiotics
The second important conclusion from this study is that the presence of Candida albicans in a weakened or disturbed gut flora actively changes its bacterial composition as it rebuilds. The researchers found that, after 21 days, the mice which had been given antibiotics exhibited dramatically lower levels of Lactobacilli bacteria, the lactic acid bacteria that are found in most probiotic supplements. The overall level of bacteria in the gut was roughly the same as the mice which had taken no antibiotics, but the composition of the gut flora was very different.
The significance of this is that these Lactobacilli (or lactic acid bacteria) are one of our best defenses against a Candida overgrowth — they lower the gut pH and prevent Candida from switching to its fungal form. By greatly reducing the numbers of this family of bacteria, Candida is able to survive more easily.
It seems that the presence of Candida albicans in a disturbed gut flora greatly affects the way that the gut flora is rebuilt. Not only does Candida colonize the gut and stay there for long periods, but it also prevents the growth of the ‘good bacteria’ most likely to prevent its colonization. Just like the way it changes the pH of its surroundings, this is an example of Candida albicans altering its environment to allow for faster growth and better colonization.
Recovering From Antibiotics And Treating A Candida Overgrowth
Antibiotics can have some wonderful uses, but always remember that they come with potential long term costs to your health. Healthy gut flora are associated with better digestion and immunity, whereas a disturbed gut flora has been linked to diarrhea, depression, gut inflammation, respiratory conditions like asthma, childhood obesity, and much more. That’s why supplementing with probiotics before and after a course of antibiotics is almost always a good idea, and certainly something that you should be discussing with your doctor.
Once Candida albicans has colonized the gut, it can be extremely difficult to shift. This is due in large part to the adaptability displayed by Candida, and the way that it creates biofilms to protect itself. Strategies like a low-sugar diet, antifungals, enzymes, and probiotics can all be helpful, but to be most effective they need to be used together. Dr Eric Wood and I have created an anti-Candida plan that includes a biofilm protocol and a strategic, multi-stage approach to beating Candida. If you’re serious about recovering from Candida overgrowth, give it a try.
References
- Vylkova et al (2011), “The Fungal Pathogen Candida albicans Autoinduces Hyphal Morphogenesis by Raising Extracellular pH”, http://mbio.asm.org/content/2/3/e00055-11.full.
- Dornward et al (2013), “Modulation of Post-Antibiotic Bacterial Community Reassembly and Host Response by Candida albicans”, http://www.nature.com/srep/2013/130712/srep02191/full/srep02191.html.

3-Month Candida Elimination Kit Start Your 3-month Candida Cleanse
This Candida Kit contains all the supplements recommended on the Candida Diet:
- LIVER ONE to process and remove the toxins created by Candida.
- CANDASSIST to inhibit and weaken the Candida colonies in your gut.
- PROBIOTIC to replace the Candida yeast with probiotic bacteria.
Plus... the CANDIDA DIET RECIPE BOOK with 50+ low-sugar recipes

I have been trying to rid my gut of candida for over 7 years. I have a nutritious who educated me about this terrible disease and I am able to manage it with Probiotics,antifungal medicatios and supplements. My condition has improved but my immune system is challenged. Any guidance for a cure?
Hello what antiviral medicine did you use
I started the diet Feb. 23, 2014 and am still following it quite closely. I have had Candida for a long time. did not know what it was called till 2 years ago when a Homeopath told me. She put me on a diet much like yours but allowed way to many carbs, fruit, and grains. We did not realize how bad the Candida was. I weighed 142 lbs when I started your diet and to date I am now 114 lbs!! I am 5 feet tall on a small frame and should weigh between 100 and 110 lbs. Almost there!! THANK YOU!
I still have the hair feeling on the back of my tongue (oral Thrush) I’m oiling (not daily) but don’t seem to have ant difference, anything else you can suggest? i can’t get your updates, something with my computer but my Mom sends them to me. Can’t wait for my Dr. appointment in June. the weight is down so pretty sure the cholesterol will be down too, and the thyroid will be higher. Dr. tried to put me on pills for both conditions but i knew there was an underlying reason for the conditions.
Thanks Again
Diana Brown
Hi, its been about 2 days now just reading about your diet programme.I v been suffering fron candida for a very long time,and it is really making my life a living hell.the viginal discharge that is smelly before and after my periods,iv had antibiotics but it still persistent.I’m really hoping your diet plan will help.
Antibiotics kill the good bacteria in your gut, leaving your body defenseless against harmful pathogens like the fast-growing Candida albicans. … Taking probiotics before, during, and after your course of antibiotics can help to maintain the balance in your digestive system. Once Candida albicans has colonized the gut, it can be extremely difficult to shift. This is due in large part to the adaptability displayed by Candida, and the way that it creates biofilms to protect itself. Strategies like a low-sugar diet, antifungals, enzymes, and probiotics can all be helpful, but to be most effective they need to be used together.
Dr.Alicia Armistead at Healing Arts NYC is helping me. I’m sure she can help you!
I didn’t know that candida overgrowth could be caused by antibiotics. I guess antibiotics really alter how your immune system operates. You can tell you have candida overgrowth if you experience frequent toe fungus.